Understanding the Gut Brain Axis & Systemic Stress
The intricate relationship between our gut and brain, known as the gut-brain axis, has garnered significant attention in recent years, particularly...
Understanding the relationship between stress and the gut microbiome is crucial for anyone researching long-term health, mental or neurological well-being, or the underpinnings of the gut–brain axis.
Scientific evidence confirms that chronic stress, psychological stress, and acute stress all impact gut microbiota composition, trigger inflammatory responses, and disrupt gut barrier integrity. This promotes dysbiosis and increasing risk for both mental health issues and gut-related disorders.
This article examines the mechanisms by which stress affects the gut microbiome, the clinical implications for conditions like irritable bowel syndrome, and how evidence-based sequencing from Cmbio empowers individuals to detect, monitor, and address stress-related disruptions to gut health.
The gut–brain axis forms a two-way communication network connecting the central nervous system (CNS) with the gut. Through neural, immune, endocrine, and metabolic signals, the brain can influence digestive function and gut microbes, while gut bacteria release molecules that alter brain chemistry and mental health. Modern research confirms that imbalances in the gut microbiome not only respond to stress but may also help shape our mood, our resilience, and our risk for disorders like depression and anxiety.
Why does this matter? The gut microbiome operates like a dynamic ecosystem, a healthy, diverse community supports optimal brain function and stress response, but disruption or "dysbiosis" in can trigger cascades of inflammation, poor gut barrier function, and altered gut brain communication and signaling to the brain amplifying mental health and neurological risks.
Cmbio specializes in advanced microbiome sequencing, integrating laboratory analysis, stress-related consultation, and multi-omics data to generate personalized, actionable recommendations. Our services enable you to:

Stress activates the hypothalamic–pituitary–adrenal (HPA) axis, leading to the release of CRH, ACTH, and cortisol. Simultaneously, the autonomic nervous system shifts toward increased sympathetic activity and reduced vagal tone, altering gastrointestinal regulation.
CRH is also released locally in the gastrointestinal tract, influencing enteric neurons, mast cells, and epithelial cells. This promotes intestinal permeability, immune activation, and neuroinflammation.
Stress-related signalling alters motility, suppresses digestive secretions, and impairs blood flow and nutrient absorption. These changes reduce gut efficiency and create conditions for functional GI disorders.
Afferent signals from the gut (including neurotransmitters, cytokines, and vagal input) influence CNS activity. This reinforces the stress response and contributes to chronic dysregulation of both emotional and gastrointestinal function.
Explore Human Health Gut Microbiome Research
Stress affects the gut microbiome in numerous ways. The most common changes include:
Both acute stress (e.g., physical stress or emotional stress) and chronic psychological stress disrupt the gut microbiome and related gut microbiota composition, causing blooms of pathogenic bacteria (often gram negative bacteria such as some Proteobacteria) and a decrease in beneficial bacteria like Lactobacillus.
In humans, academic and psychosocial stressors reduce gut microbiota diversity, alter gut bacterial composition, and increase the prevalence of potentially harmful bacteria. Examples include students under academic stress or adults experiencing chronic psychosocial stress and trauma.
Chronic stress, including social stressor alters and early life stress, primes the microbiota gut brain axis for mood disorders and can lead to lasting shifts in the gut microbiota and immune system interactions.
Stress increases gut permeability (“leaky gut”), allowing bacterial fragments and endotoxins to enter circulation, which triggers an inflammatory response. Short-term psychological stress and chronic stressors both disrupt gut barrier function by affecting gut epithelial cells and mucosal lining.
This leaky gut phenomenon has been observed following emotional stress, chronic marital conflict, and experimentally after public speaking stressors.
Gut motility and digestive efficiency become unstable under stress. Disruption of neural, hormonal, and immune signals alters gut movement and the production of protective mucus, often resulting in:
|
Feature |
Healthy/Low-Stress State |
Chronic/Acute Stress State |
|
Microbial Composition |
High gut microbiota diversity; abundance of beneficial bacteria (Lactobacillus, Bifidobacterium); balanced ratio of commensal microbes |
Reduced gut microbiota diversity; bloom of pathogenic or pro-inflammatory bacteria (e.g., Proteobacteria, Escherichia/Shigella); diminished beneficial strains; altered gut microbial composition |
|
Barrier Integrity |
Intact gut barrier; tight junctions maintained; low gut permeability (“leaky gut” is rare); efficient segregation of gut bacteria from bloodstream |
Increased gut permeability (“leaky gut”); disrupted tight junctions in gut epithelial cells; more bacterial endotoxins and fragments leak into the bloodstream; triggers systemic inflammation and local immune activation |
|
Digestion Changes |
Stable digestion; efficient absorption of nutrients; balanced gut motility; robust production of short-chain fatty acids |
Altered digestion; unpredictable or unstable gut motility (diarrhea/constipation); decreased short-chain fatty acid production; impaired nutrient absorption; increased digestive symptoms (e.g., bloating, pain) |
Early life stress or stress exposure early in development can imprint lasting changes on the microbiota gut brain axis, increasing the risk of mood disorders, autism spectrum disorders, and irritable bowel syndrome later in life.
Recent studies reveal that the microbiota and stress induced responses follow circadian rhythms, so time of day impacts both diagnosis and intervention outcomes.
Bottom line: Stress-induced alterations in the gut microbiome are systematic and multifaceted, they compromise beneficial microbial balance, weaken gut barrier integrity, and destabilize digestion. These negative effects not only endanger gut health but have downstream impacts on immunity, mood, and risk for chronic disorders.
Key takeaways include:
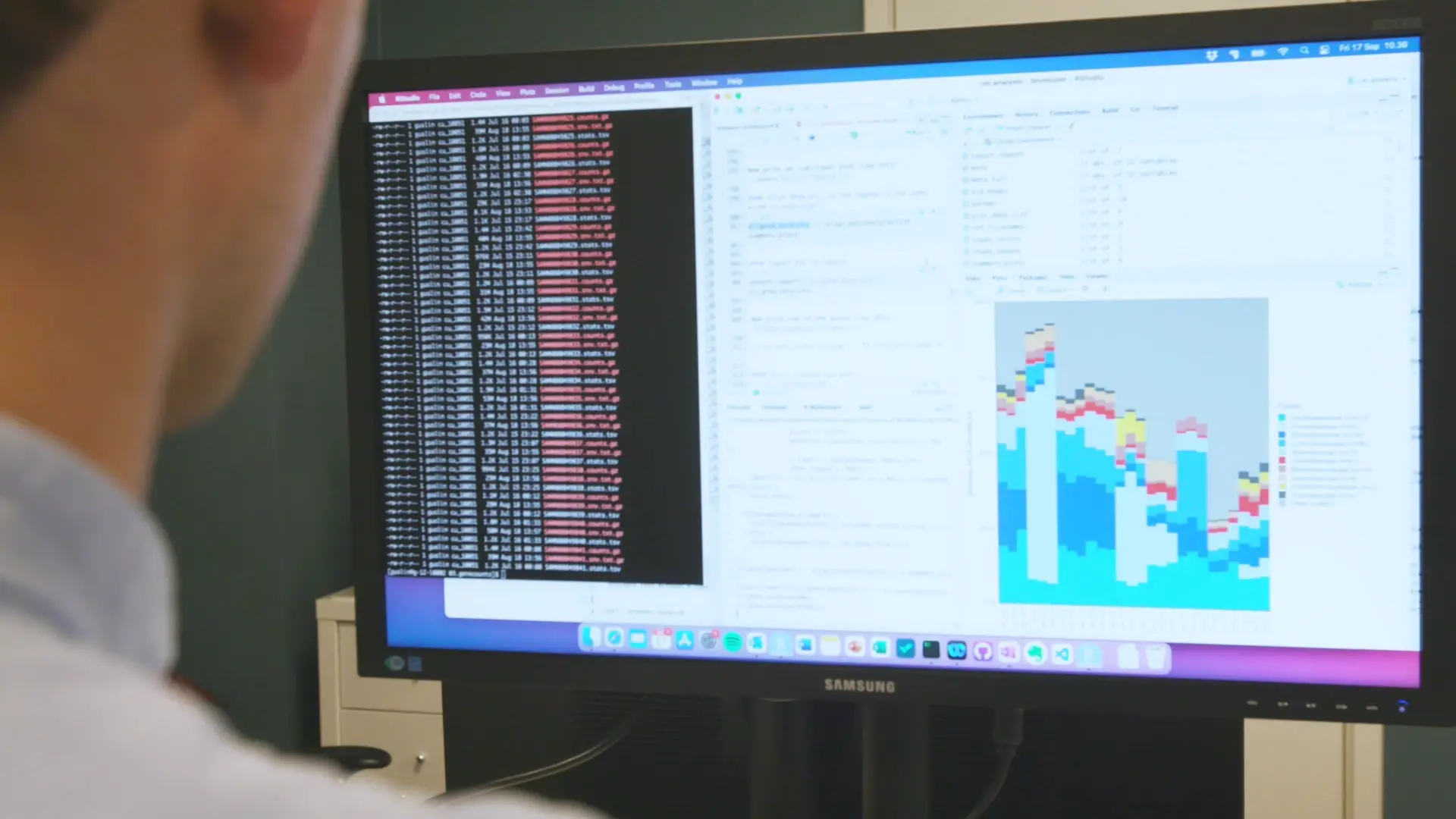
Cmbio’s comprehensive sequencing and stress integrated analysis enables precise tracking of dysbiosis, gut microbial composition, and strain-level disruptions including in inflammatory bowel disease, major depressive disorder, and gut brain axis related conditions.
Our research-driven, state-of-the-art approach provides the tools to monitor, understand, and reverse these changes, supporting resilience, healthy gut function, and optimal mental health.
Explore Human Health Gut Microbiome Research and Neurology and Mental Health Microbiome Research to begin your journey to a healthier mind and body.
The intricate relationship between our gut and brain, known as the gut-brain axis, has garnered significant attention in recent years, particularly...
Grabrucker S, Marizzoni M, Silajdžić E, et al. Microbiota from Alzheimer’s patients induce deficits in cognition and hippocampal neurogenesis....

Celiac Disease, an autoimmune intestinal disorder affecting an estimated1%of the population, is characterized by the body’s inappropriate response...